A debate over the future of Scotland’s health service is now underway. The Scottish Government says it now backs a “national conversation” on the future of the NHS. As BMA Scotland has set out, reform is essential if the NHS is to survive.
But what does reform involve? Our Scottish Future will be examining the future of healthcare in Scotland this year as the debate gets underway. In our view, reform means embracing the explosion in health tech and health innovation as the best way to improve Scotland’s health and thereby reduce demand on primary and secondary care. Furthermore, we believe – and can show – that this transformation in health is best done when researchers and clinicians in Scotland, England, Wales and Northern Ireland join forces to accelerate the pace of change.
This year, we will be setting out detailed ideas. This first blog of 2024 sets out our thinking on where the NHS stands in Scotland and how the adoption of the “3Ps” can keep it sustainable in the long-term.
—————————————————————————————————————————-
By Jonathan Doogan, David Kerr, Dec Doogan, Eddie Barnes
The UK/ Scottish National Health Service (NHS) is in many respects the envy of the world. Open to all citizens, free at the point of delivery, and (in theory) equitable care for all. However, from a human, societal and fiscal perspective, it is severely challenged. An urgent and radical re-imagining of the Scottish NHS is required.
Scotland has often been labelled ‘the sick man of Europe’ due to higher mortality rates compared with other western European countries. Life expectancy in Scotland is the lowest in Western Europe; it has the lowest life expectancy of all UK countries for both males and females.
There are huge inequalities driven by location in Scotland. Life expectancy for men in the most deprived regions of Scotland are 13 years less than the most affluent. In the most deprived areas, men and women spend more than a third of their life in poor health.
UK and Scottish Health outcomes are challenged, e.g. rates of death following Myocardial Infarction (MI) are higher than other developed OECD nations. Scotland has highest overall mortality for cancer in the UK. In Scotland, mortality from cancer for both sexes was about 15% higher than in the UK as a whole, and the incidence of cancer was 10% higher.
Scottish Govt spending on health and social care for a population of 5.5m people was £19.2bn in 2023 (just under 20% of total government expenditure), although Scottish health spending per person now only 3% higher than in England, compared with 22% at the start of devolution.
The Scottish NHS is not a health service at all; it is a National Sickness Service. The vast majority of the focus is on tackling disease diagnosis and treatment.
There is insufficient focus on Prevention of disease, where the greatest return on investment would be realised at a financial and human level. There is an opportunity to Personalise healthcare across the patient journey to ensure greater empowerment and engagement of people in their own healthcare. Data and technology innovation will enable ever greater precision in delivery of treatment to improve individual outcomes and system efficiency.
In order to do so, we need a NHS, which places the individual at the centre – with an enhanced focus Prevention, Precision and Personalisation of care. Placing peoples’ (not just patients) full life journey at the centre of a genuinely patient-centric NHS.
The patient journey: the full life journey from birth to death
Building a healthcare system around the needs of individual people/ patients is not easy – but we are better placed now than ever to do so.
We first need to look at the “full-life journey” of people and patients across their lifetime from birth to death. This is across all demographic, geographic and behavioural segments. There are learnings here from consumer-centric organisations and companies which have individualised, consumer-centric business models and systems (e.g. grocery, financial services, consumer goods).
The Scottish population is broad and diverse. Developing a healthcare system which is more individualised, more bottom-up (patient-centric) than top-down (system-centric) is a significant challenge. However, much of disease and the associated human and societal cost is predictable. In a world of emerging “big”, “real world” data, we are able to understand, and in many cases predict, what diseases will likely develop.
There is huge value in a prevention-oriented health service but it will require the harnessing of available data sources (traditional and new), and the development of and application of powerful new predictive tools, built upon integrated data platforms.
The increased focus on prevention will not fully prevent disease. The system needs to be set-up for early detection and diagnosis, and for precision treatment and personalised healthcare to prevent relapse and recurrence of devastating and costly health events.
Four key challenges will need to be addressed in order to implement such a model and realise this value. First, is culture and mindset: placing people/ patients at the centre and not just treat disease. Second, is data integration, this has both technical and cultural/ organisational components. Third, is patient engagement and empowerment, placing data in the hands of the population around their own healthcare – and create incentives to drive behaviour change. Fourth, is the creation of a truly collaborative environment of value-based “ecosystem” partnerships. This will require the engagement of both integrated healthcare services to utilise new data sources and emerging technology platforms and solutions. It will also require a well-trained, motivated and appropriately incentivised and joined-up workforce.
Prevention, Precision & Personalisation: shift from National Sickness Service to National Health Service by 2035
Healthcare should be viewed as an investment not a cost. An investment in people and the future prosperity of the nation.
The route to this more desirable future state is viewed through the lens of: Prevention, Precision and Personalisation “3Ps” (see figure 1 below). We need to mine deep into the People/Patient journey, and the critical pain points (e.g. inaccurate diagnosis, inappropriate referral and treatment, lack of adherence) where most value can be realised. This will require the utilisation of individualised real world data, HC system integration and patient engagement.
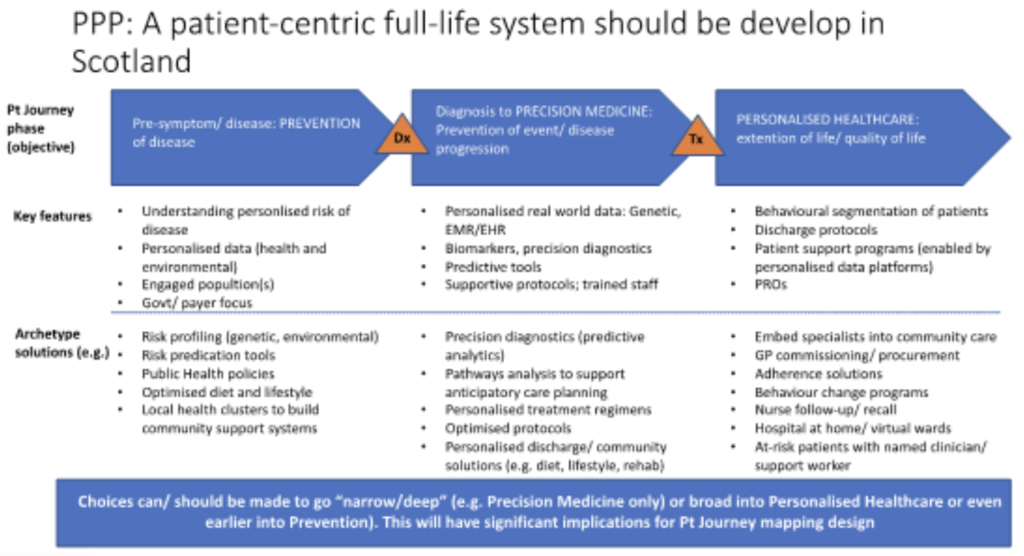
Figure 1: Patient life journey: Prevention, Precision, Personalisation (source: Our Scottish Future)
The solutions required to meaningfully impact these critical patient journey pain points will require focus on developing existing and new partnerships in the broader healthcare “ecosystem”. Many of these solutions exist today and are improving and scaling at pace, for example, precision therapeutics and diagnostics, predictive/ AI algorithms, personalised health dashboards and applications.
This new model will be made up of existing partners (payers, providers, policy makers) and new stakeholders (patients, technology, insurance, financial services, grocery) – all built around the existing NHS. The NHS needs to become a world-class partner to valuable existing and new organisations.
The future is possible. There are “lighthouse” health systems to learn from: Singapore, Finland, Estonia, Israel where data, system integration, prediction and patient empowerment are design features and outcomes and efficiency are orders of magnitude higher than in Scotland. Countries like Australia, Canada and The Netherlands can also offer inspiration. Closer to home, there are numerous pockets of best practice across the UK that should be selectively prioritised and scaled – there is a major opportunity to build upon of real-world data platforms in UK.
The future model will not be a monolithic national health service, but a tiered, tailored and personalised system for all. This will be a national and public system, blended with valuable overlays, channels and services which come from new, potentially private, partners and organisations.
The new model should be a radical re-envisioning of the current NHS, with disruptive and complementary solutions and built on x-sector partnership. The goal has to be on producing fundamentally better outcomes for individuals and the population, and avoiding massive costs to the system. It is a Value-based National Health Service.
Jonathan Doogan is an independent healthcare and biotech consultant. He is the former European Head of Digital Innovation at Amgen and Novartis, and is a healthcare industry advisor at Oxford University.
David Kerr is professor of cancer medicine at Oxford University and is the chair of the National Framework for Service change in NHS Scotland
Dec Doogan is a visiting professor at Glasgow University and a fellow of the Royal College of Physicians and Surgeons of Glasgow. He has more than 30 years experience in the global pharmaceutical industry. He is Chairman and co-founder of Biohaven Pharmaceuticals
Eddie Barnes is director of Our Scottish Future
APPENDIX
Sources and links: available data/ reports
Figure 1: Disease-agnostic, health outcome-focused model (source: From: A Narrative Review of the Patient Journey Through the Lens of Non-communicable Diseases in Low- and Middle-Income Countries)
Similar thesis: https://www.openaccessgovernment.org/turning-the-national-illness-service-into-the-national-health-service/109395/
Report: https://www.gov.scot/publications/scottish-health-survey-2021-volume-1-main-report/pages/4/
Report on HC attitudes: https://natcen.ac.uk/news/scottish-health-survey-reveals-decline-wellbeing-pandemic
Report Patient survey: https://www.gov.scot/publications/health-care-experience-survey-2021-22-national-results/
Report Scottish data: https://www.scdi.org.uk/policy/mindthegap/
Scottish Data: https://www.nhsresearchscotland.org.uk/research-in-scotland/data/health-informatics
Scottish HER Data: https://www.nhsresearchscotland.org.uk/research-in-scotland/data/sub-page-4
Example solutions for the new world
Example personalised health apps: https://digi.me
Example: RWE data integration https://aetion.com
Example Predictive algorithms: https://www.philips.com/a-w/about/news/archive/features/20200604-predictive-analytics-in-healthcare-three-real-world-examples.html
Example Predictive algorithms in CV: https://owkin.com/publications-and-news/press-releases/owkin-and-amgen-use-ai-to-improve-cardiovascular-risk-prediction
Example Predictive algorithms: https://acrabstracts.org/abstract/early-and-accurate-diagnosis-of-patient-with-axial-spondyloarthritis-using-machine-learning-a-predictive-analysis-from-electronic-health-records-in-united-kingdom/
Health and wellbeing apps: https://www.goodhousekeeping.com/health-products/g4841/health-apps/